Colon Resection Surgery: What to Expect, Long-Term Effects, and Life After Surgery

Colon Resection Surgery: What to Expect, Long-Term Effects, and Life After Surgery Colon resection, medically known as colectomy, is a surgical procedure to remove part or all of the colon. This intervention is often necessary for treating conditions like colorectal cancer, diverticulitis, inflammatory bowel diseases (IBD), and severe intestinal obstructions. While this surgery can be life-saving, it comes with challenges and lifestyle changes. This article provides a detailed understanding of the procedure, its potential long-term side effects, and insights into life expectancy after colon resection. What is Colon Resection? Colon resection involves removing the damaged or diseased segment of the colon. Depending on the patient’s condition, surgeons may reconnect the healthy parts of the colon (primary anastomosis) or create a temporary or permanent stoma (colostomy). Types of Colon Resection Partial Colectomy: Removal of only the affected part of the colon. Total Colectomy: Removal of the entire colon, sometimes required for extensive disease. Hemicolectomy: Removal of the left or right side of the colon. Proctocolectomy: Removal of both the colon and rectum, often used for certain cancers or severe IBD cases. Why is Colon Resection Necessary? The decision to undergo colon resection is typically based on the severity of the underlying condition. Common indications include: Colorectal Cancer: The most common reason for colon resection. Removing the tumor and nearby lymph nodes is essential to prevent the spread of cancer. Diverticulitis: Chronic or recurrent diverticulitis may necessitate surgery to avoid complications like perforations or abscesses. Inflammatory Bowel Diseases: Conditions such as Crohn’s disease or ulcerative colitis often lead to severe damage requiring resection. Bowel Obstructions: When non-surgical methods fail to alleviate blockages caused by tumors, scar tissue, or volvulus. The Surgical Process Preoperative Preparation Patients may undergo various tests such as blood work, imaging studies, and a colonoscopy. A bowel cleansing regimen is typically required before surgery. Your surgeon will discuss the type of resection, anesthesia, and recovery expectations. During Surgery Colon resection can be performed using two techniques: Open Surgery: Involves a larger incision for direct access to the colon. Laparoscopic Surgery: A minimally invasive approach using small incisions and a camera for guidance. Postoperative Care Post-surgery, patients are monitored for signs of infection, bowel function, and overall recovery. Most patients begin with a liquid diet and gradually reintroduce solid foods Long-Term Side Effects of Colon Resection Surgery While many individuals recover well after colon resection, some may experience long-term effects that can impact their quality of life. Changes in Bowel Habits Frequent Bowel Movements: After resection, the remaining colon may have reduced capacity to absorb water, leading to loose stools. Constipation or Diarrhea: Depending on the extent of surgery and the individual’s response, bowel patterns can vary significantly. Nutritional Deficiencies The colon plays a role in absorbing certain nutrients. After resection, some patients may experience deficiencies in vitamins and minerals, especially if a significant portion of the colon is removed. Adhesions and Obstructions Scar tissue can develop, causing bowel adhesions that may lead to partial or complete obstructions. Risk of Recurrence In cases of cancer or inflammatory bowel diseases, there’s a potential for disease recurrence, requiring regular follow-ups and screenings. Emotional and Psychological Impact Adjusting to life after surgery, especially if a stoma is involved, can be emotionally challenging. Support groups and counseling can be beneficial. Life After Colon Resection Recovery and Rehabilitation Recovery from colon resection varies based on factors such as the extent of surgery, the patient’s age, and overall health. Most individuals resume normal activities within 4-6 weeks. Dietary Adjustments Balanced Diet: A diet rich in fiber, lean protein, and essential vitamins can help manage bowel function. Avoid Trigger Foods: Foods that cause gas, bloating, or diarrhea should be avoided initially. Hydration: Staying well-hydrated is critical to compensate for reduced water absorption by the colon. Physical Activity Gradual reintroduction of physical activity is encouraged to prevent complications like blood clots and promote overall health. Stoma Care (if applicable) For those with a colostomy, proper stoma care is essential to prevent infections and maintain hygiene. An ostomy nurse can provide guidance and support. Life Expectancy After Colon Resection Colon resection can significantly improve life expectancy, particularly for patients with cancer or severe bowel diseases. Factors influencing life expectancy include: Underlying Condition: Early-stage cancers treated with resection have a better prognosis than advanced stages. Surgical Success: A successful surgery with minimal complications enhances recovery and long-term outcomes. Post-Surgery Lifestyle: Maintaining a healthy lifestyle, including regular exercise and a nutritious diet, plays a pivotal role in longevity. Follow-Up Care: Regular check-ups, including colonoscopies, help monitor for recurrence or complications. While life expectancy varies from person to person, many patients go on to lead full and active lives following surgery. Tips for Managing Long-Term Effects Regular Medical Check-UpsMonitor for signs of recurrence, obstructions, or other complications with routine follow-ups. Adopt a Healthy LifestyleA balanced diet, regular exercise, and stress management are vital for overall well-being. Stay InformedUnderstanding your condition and its management can empower you to make informed decisions about your health. Seek SupportJoin support groups for individuals recovering from colon resection. Sharing experiences can provide emotional and practical guidance. Conclusion Colon resection surgery is a critical intervention that can save lives and improve the quality of life for many individuals. While the procedure comes with potential challenges, such as long-term side effects of colon resection surgery, most patients can adapt and lead fulfilling lives with proper care and lifestyle adjustments. For those wondering about life expectancy after colon resection, the outlook is generally positive, especially when the surgery addresses treatable conditions like early-stage cancer or localized bowel disease. With advancements in surgical techniques and post-operative care, the journey toward recovery is more manageable than ever before. By staying proactive, embracing lifestyle changes, and following medical advice, patients can look forward to a healthy and active future post-surgery. Frequently Asked Questions (FAQs) About Colon Resection Surgery What is colon resection surgery? Colon resection, or colectomy, is a surgical procedure to remove part or all of the colon. It is often
Understanding Cancer Fatigue: A Comprehensive Guide for Cancer Patients
Understanding Cancer Fatigue: A Comprehensive Guide for Cancer Patients Cancer fatigue is one of the most common and debilitating symptoms experienced by people undergoing cancer treatment. It’s different from the normal tiredness everyone experiences, often lingering and not relieved by sleep. This type of fatigue can affect a patient’s ability to function daily, making it one of the most challenging aspects of cancer treatment. Understanding its causes, symptoms, and ways to manage it is essential for both patients and caregivers. What Is Cancer Fatigue? Cancer fatigue refers to an overwhelming feeling of tiredness or exhaustion that doesn’t go away with rest or sleep. It is often seen in patients undergoing chemotherapy, radiation, or even those recovering from surgery. Unlike regular fatigue, cancer fatigue may make it difficult to carry out simple tasks, such as getting out of bed, walking, or eating. The Main Characteristics of Cancer Fatigue: Persistent: Doesn’t improve with rest. Physical and mental exhaustion: Affects both body and mind. Interferes with daily life: Makes it hard to perform normal activities. Unpredictable: Its intensity can vary, sometimes becoming overwhelming. Why Does Cancer Cause Fatigue? Cancer fatigue can result from several factors, many of which are related to the cancer itself or its treatments. The most common reasons include: Cancer Treatments: Chemotherapy, radiation, and surgery can all lead to physical fatigue, as they damage healthy cells and tissues. Cancer-Related Stress: The emotional strain of dealing with a cancer diagnosis can lead to mental exhaustion. Anemia: A decrease in red blood cells can result in less oxygen being transported throughout the body, leading to tiredness. Pain and Discomfort: Chronic pain can drain energy and make it hard to sleep or relax. Poor Sleep: Stress, pain, and side effects of treatment can disrupt sleep patterns, leading to increased fatigue. Nutritional Deficiencies: Cancer and its treatments can cause a loss of appetite, resulting in poor nutrition, which can contribute to fatigue. Symptoms of Cancer Fatigue Cancer-related fatigue manifests in various ways, and it’s not always the same for every patient. Common symptoms include: Feeling tired or drained, even after a full night’s rest. Difficulty concentrating or focusing. Lack of energy, making even small tasks feel exhausting. Increased need for naps throughout the day. Reduced interest in social activities or hobbies. Weakness or lack of physical stamina. Managing Cancer Fatigue While cancer fatigue can be overwhelming, there are several strategies to help manage and reduce its impact. Working with your healthcare team to develop an individualized plan is key. Here are some common approaches: Rest and Sleep Getting adequate sleep is vital, although it may not completely eliminate fatigue. Establishing a regular sleep routine, keeping the sleep environment calm, and avoiding stimulants like caffeine can help improve sleep quality. Exercise Gentle physical activities such as walking, stretching, or yoga can help improve energy levels and combat fatigue. Always consult your doctor before starting an exercise routine to ensure it’s safe based on your condition and treatment. Nutrition Maintaining a balanced diet is crucial for cancer patients. A diet rich in fruits, vegetables, proteins, and whole grains can help combat fatigue. Sometimes, a nutritionist may suggest supplements if deficiencies are present. Stress Management Cancer-related fatigue can be worsened by emotional and mental stress. Practicing relaxation techniques such as deep breathing, meditation, or mindfulness can help manage stress and improve overall well-being. Medications In some cases, medications may be prescribed to help manage fatigue, especially if anemia or other underlying conditions are contributing to the tiredness. Support Systems Having a support system in place can ease the emotional burden of fatigue. Whether it’s family, friends, or a support group, having people to lean on can reduce stress and help manage feelings of isolation. Pacing Yourself It’s important for cancer patients to listen to their bodies and pace themselves. Trying to accomplish everything at once can worsen fatigue. Breaking tasks into smaller steps and resting between activities can help manage energy levels. The Importance of Communication If you’re experiencing severe fatigue, it’s crucial to talk to your healthcare team. They can help assess the cause of your fatigue and provide solutions that are tailored to your specific needs. Sometimes, fatigue can be a sign of something more serious, such as anemia or an infection, so early intervention is essential. Conclusion Cancer fatigue is a complex and often debilitating symptom that can affect all aspects of a cancer patient’s life. However, it’s important to understand that it is manageable. With the right strategies, including proper rest, nutrition, exercise, and support, you can significantly improve your energy levels and quality of life during your cancer journey. If you’re struggling with cancer fatigue, don’t hesitate to talk to your healthcare team. Together, we can create a plan that works for you, helping you regain the energy you need to enjoy life to the fullest. For more information on cancer care, treatment, and support, visit Pi Health Cancer Hospital. FAQS About Cancer Fatigue How can I tell if my fatigue is related to cancer or something else? Cancer fatigue often doesn’t improve with rest and can be accompanied by other cancer-related symptoms. If you’re unsure, speak with your healthcare provider to rule out other potential causes. Can cancer fatigue be treated? Yes, cancer fatigue can be managed with a combination of strategies, including rest, exercise, diet, and medication. Your healthcare team can work with you to find the best approach. Is cancer fatigue different from regular tiredness? Yes, cancer fatigue is much more intense, persistent, and not relieved by sleep or rest. It can affect your physical and mental capacity to function on a daily basis. Does everyone with cancer experience fatigue? Not everyone with cancer will experience fatigue, but it is a very common side effect, especially during or after treatment. Can I prevent cancer fatigue? While it might not be possible to prevent cancer fatigue entirely, maintaining a healthy lifestyle, managing stress, and staying physically active can help reduce its severity. How long does cancer fatigue last? The
Unresectable vs Metastatic Cancer: What’s the Difference and Why Does It Matter?
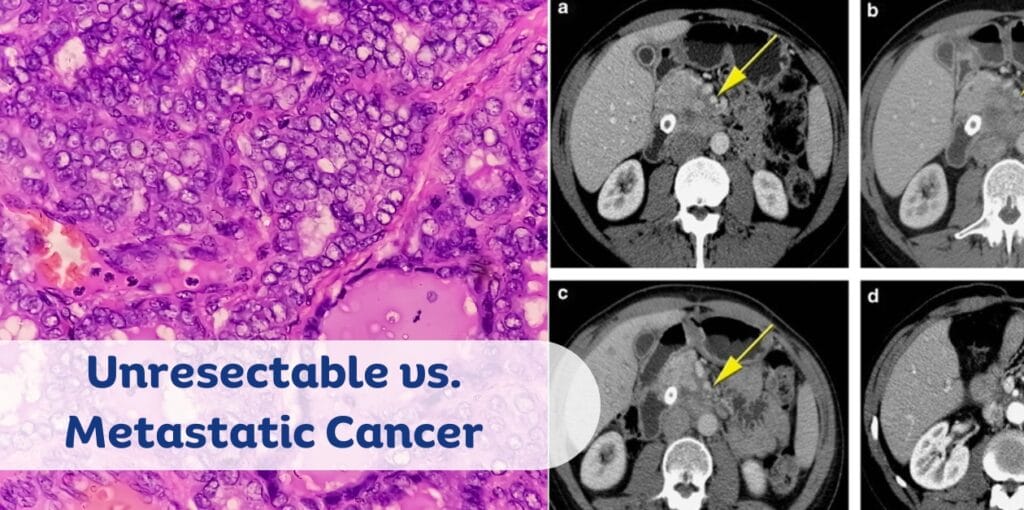
Unresectable vs Metastatic Cancer: What’s the Difference and Why Does It Matter? Cancer remains one of the most challenging diseases to treat, with various stages and classifications influencing the approach to care. Two terms often encountered in the diagnosis of advanced cancer are unresectable cancer and metastatic cancer. While these terms are related to cancer in advanced stages, they describe different aspects of the disease, each with its own treatment strategies and prognosis. Understanding the difference between unresectable cancer and metastatic cancer is crucial for patients, caregivers, and healthcare professionals. This blog will explore these terms in detail, with a special focus on the groundbreaking clinical trials conducted at PI Health Cancer Hospital under the leadership of Dr. Venugopal Arroju, Clinical Director & HOD of Medical Oncology. We’ll also examine how innovative treatments like Tislelizumab are shaping the future of cancer care. What is Unresectable Cancer? Unresectable cancer refers to tumors that cannot be removed by surgery due to their size, location, or involvement with nearby vital structures. In some cases, the tumor may be in an area that is difficult to access, such as the lungs, liver, or spine, making surgical intervention risky or technically impossible. Unresectable cancer typically indicates an advanced stage, but it does not always mean that the cancer has spread to other parts of the body. Key Features of Unresectable Cancer: Surgical intervention is not possible due to the tumor’s size, location, or involvement with nearby structures. Treatment focuses on shrinking the tumor, slowing its growth, and improving symptoms through therapies like chemotherapy, radiation therapy, and immunotherapy. The prognosis for unresectable cancer can vary depending on the type of cancer, its growth rate, and how well it responds to treatment. What is Metastatic Cancer? Metastatic cancer, on the other hand, refers to cancer that has spread beyond its primary (original) location to distant parts of the body. This process, known as tumor spread, can occur through the bloodstream or lymphatic system. As cancer cells travel to other organs, they form secondary tumors, which can make treatment more complex. Metastatic cancer is often considered to be at an advanced stage (stage IV) and is typically harder to treat because it affects multiple organs. Key Features of Metastatic Cancer: Tumor spread to other parts of the body (lungs, liver, bones, or brain). Cancer stages play a critical role in diagnosing metastatic cancer, with stage IV signifying widespread spread. Treatment strategies for metastatic cancer often involve a combination of chemotherapy, radiation therapy, targeted therapy, and immunotherapy, and focus on controlling the disease and improving the patient’s quality of life. Unresectable Cancer vs. Metastatic Cancer: Key Differences The main distinction between unresectable cancer and metastatic cancer lies in the nature of the tumor’s spread and the approach to treatment: Factor Unresectable Cancer Metastatic Cancer Definition Tumors that cannot be surgically removed. Cancer that has spread from its primary site. Surgical Intervention Surgical Intervention Surgery is not an option. Surgery may be considered for isolated cases. Surgery may be considered for isolated cases. Treatment Options Chemotherapy, radiation, immunotherapy. Chemotherapy, immunotherapy, targeted therapy. Prognosis Prognosis varies based on tumor type and response to treatment. Prognosis often poorer, as cancer affects multiple organs. Cancer Stages Typically diagnosed at an advanced stage but not necessarily metastatic Stage IV cancer, indicating metastasis. Treatment Options for Unresectable and Metastatic Cancer Unresectable Cancer Treatment: The treatment for unresectable cancer often focuses on reducing the size of the tumor and controlling the disease through nonsurgical means. These options include: Chemotherapy: A systemic treatment that uses drugs to destroy cancer cells or stop their growth. Radiation Therapy: High-energy rays are used to target and kill cancer cells. Immunotherapy: Drugs like Tislelizumab (an immune checkpoint inhibitor) are increasingly being used to treat unresectable cancers. Tislelizumab works by enhancing the immune system’s ability to recognize and destroy cancer cells. Targeted Therapy: This approach targets specific genes or proteins that contribute to cancer growth. Metastatic Cancer Treatment: Metastatic cancer requires more comprehensive treatment strategies due to the spread of cancer to multiple parts of the body. Treatment often includes: Chemotherapy: To treat cancer cells in various organs. Immunotherapy: Tislelizumab is one of the most promising treatments in metastatic cancer care, helping the immune system fight cancer cells, especially in hard-to-treat areas. Targeted Therapy: Targeting specific mutations in the cancer cells to halt their growth and spread. Palliative Care: For advanced metastatic cases, the focus may shift toward relieving symptoms and improving the quality of life. Groundbreaking Clinical Trials at PI Health Cancer Hospital Metastatic cancer PI Health Cancer Hospital, under the leadership of Dr. Venugopal Arroju, has been at the forefront of innovative cancer treatments, especially in the field of immunotherapy. Clinical trials focusing on Tislelizumab have shown promising results, offering new hope for patients with both unresectable and metastatic cancers. Dr. Venugopal Arroju, an experienced oncologist and medical director at the hospital, has led various clinical trials exploring the efficacy of Tislelizumab for patients who have not responded to traditional treatments. This breakthrough immunotherapy drug has shown significant potential in improving patient outcomes, prolonging survival, and even shrinking tumors in certain cases. PI Health’s Contribution to Cancer Research: Immunotherapy Advancements: The hospital’s research in Tislelizumab has opened new doors in immuno-oncology, especially in treating unresectable and metastatic cancers. Patient-Centric Approach: Clinical trials at PI Health Cancer Hospital emphasize personalized treatments, aiming to improve each patient’s prognosis based on the specific nature of their cancer. requires more comprehensive treatment strategies due to the spread of cancer to multiple parts of the body. Treatment often includes: Chemotherapy: To treat cancer cells in various organs. Immunotherapy: Tislelizumab is one of the most promising treatments in metastatic cancer care, helping the immune system fight cancer cells, especially in hard-to-treat areas. Targeted Therapy: Targeting specific mutations in the cancer cells to halt their growth and spread. Palliative Care: For advanced metastatic cases, the focus may shift toward relieving symptoms and improving the quality of life. Conclusion The distinction between unresectable cancer and metastatic cancer
Rising Breast Cancer Rates in India: Awareness and Screening Are Key

Rising Breast Cancer Rates in India: Awareness and Screening Are Key Breast cancer rates are increasing across India, with Karnataka alone reporting 14,484 new cases and 5,388 deaths in 2023. Modifiable risk factors such as obesity, alcohol consumption, and hormonal prescriptions contribute to this rising trend. Early detection is crucial, with screenings recommended from age 40, or earlier for high-risk individuals, using mammograms, ultrasounds, and MRIs. Understanding the Risk Factors Breast cancer can affect anyone, but certain factors increase the risk: Non-Modifiable Factors: Age over 50, genetics, and family history. There’s also a slight increase in cases among women under 50 due to various reasons. Modifiable Factors: Obesity, alcohol intake, hormonal prescriptions, breastfeeding practices, age of childbirth, and age of menstruation. Delaying childbirth beyond 35 years and starting menstruation before age 12 can slightly increase the risk. Early Signs to Watch For Early detection of breast cancer significantly improves treatment outcomes. Be aware of these symptoms: Painless or painful lump in the breast or underarm Changes in breast shape Skin changes like dimpling or thickening Bloody nipple discharge Nipple inversion Importance of Regular Screening Screening should begin at age 40 for all women, and earlier for those with high-risk factors. Regular clinical breast examinations and self-examinations are essential, especially in areas with limited access to mammography. Screening Methods Mammogram: A non-invasive, cost-effective, and painless tool for both screening and diagnosis. It involves compressing the breast tissue between two plates to capture X-ray images. Ultrasound: Often used alongside mammograms to evaluate abnormalities, especially in younger women or during pregnancy. MRI: Recommended for patients at higher risk of developing breast cancer. Reducing Your Risk Adopting a healthy lifestyle can help reduce the risk of breast cancer: Maintain a healthy diet and weight Stay physically active Avoid smoking and limit alcohol consumption Promote breastfeeding for an adequate period Avoid unnecessary hormone therapy Take Action Today Early detection and treatment are key to fighting breast cancer. At PI Health Cancer Hospital, we offer comprehensive screening and treatment options tailored to your needs. Contact us today at +91 92814 48102 or visit our website to schedule your screening and learn more about how we can support you in your health journey. Don’t wait—early detection saves lives. Reach out to PI Health Cancer Hospital for your screening and consultation today! Dr. A. Venugopal Clinical Director & HOD Medical Oncology Senior Consultant Medical Oncologist & Hemato-Oncologist View Profile About Author Dr. A. Venugopal MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland). Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology. Book an Appointment
Demystifying the Menstrual Cycle: A Detailed Exploration

Demystifying the Menstrual Cycle: A Detailed Exploration The menstrual cycle is a fundamental aspect of female reproductive health, yet it remains shrouded in mystery and misconceptions for many. Understanding the menstrual cycle is crucial not only for reproductive health but also for overall well-being. This detailed exploration aims to demystify the menstrual cycle, breaking down its phases, hormonal changes, and the importance of menstrual health. What is the Menstrual Cycle? The menstrual cycle is a monthly series of changes that a woman’s body undergoes to prepare for the possibility of pregnancy. It typically lasts about 28 days, although it can range from 21 to 35 days in different women. The cycle is divided into several phases, each characterized by specific hormonal changes and physiological processes. Phases of the Menstrual Cycle Menstrual Phase: Duration: 3-7 days Description: This phase marks the beginning of the cycle. It involves the shedding of the uterine lining (endometrium), resulting in menstrual bleeding. This occurs if the egg released in the previous cycle is not fertilized. The menstrual phase is often accompanied by symptoms such as cramps, bloating, and mood swings. Follicular Phase: Duration: Approximately 14 days (varies) Description: Following menstruation, the body enters the follicular phase. The pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the ovaries to produce follicles. Each follicle contains an immature egg. One follicle will mature and prepare for ovulation. During this phase, estrogen levels rise, leading to the thickening of the uterine lining. Ovulation Phase: Duration: 24-48 hours Description: Ovulation occurs around the midpoint of the cycle. The mature follicle releases an egg into the fallopian tube. This phase is triggered by a surge in luteinizing hormone (LH). Ovulation is the most fertile period of the cycle, and some women may experience mild discomfort or spotting. Luteal Phase: Duration: 14 days Description: After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone. This hormone prepares the uterine lining for a potential pregnancy. If the egg is not fertilized, the corpus luteum breaks down, leading to a drop in progesterone levels and the start of menstruation. The luteal phase can be marked by symptoms of premenstrual syndrome (PMS), such as mood swings, fatigue, and breast tenderness. Hormonal Changes The menstrual cycle is regulated by a complex interplay of hormones, including: Estrogen: Promotes the growth of the uterine lining and regulates the release of FSH and LH. It peaks during the follicular phase and drops after ovulation. Progesterone: Stabilizes the uterine lining and prepares it for implantation. It rises during the luteal phase and drops if pregnancy does not occur. Follicle-Stimulating Hormone (FSH): Stimulates the growth of ovarian follicles. It is highest at the beginning of the follicular phase. Luteinizing Hormone (LH): Triggers ovulation and the formation of the corpus luteum. It surges just before ovulation. Importance of the Menstrual Cycle Understanding the menstrual cycle is vital for several reasons: Reproductive Health: Regular cycles indicate a healthy reproductive system, while irregularities can signal underlying health issues such as hormonal imbalances, thyroid disorders, or polycystic ovary syndrome (PCOS). Fertility Awareness: Knowing the phases of the cycle can help in planning or preventing pregnancy. Tracking ovulation can be particularly useful for those trying to conceive. Overall Health: Menstrual health can reflect overall well-being, as hormonal imbalances can affect various aspects of health, including mood, energy levels, and skin condition. Common Menstrual Disorders Several disorders can affect the menstrual cycle, causing discomfort and health issues. Some common menstrual disorders include: Dysmenorrhea: Painful menstruation, often involving severe cramps. It can be primary (without an underlying condition) or secondary (caused by conditions like endometriosis or fibroids). Menorrhagia: Heavy menstrual bleeding that can interfere with daily activities. It may be caused by hormonal imbalances, uterine fibroids, or other medical conditions. Amenorrhea: The absence of menstruation, which can be primary (never having menstruated) or secondary (missing periods for three or more months). Causes can include hormonal imbalances, excessive exercise, or significant weight loss. Premenstrual Syndrome (PMS): A group of symptoms, including mood swings, bloating, and irritability, that occur before menstruation. Severe PMS can interfere with daily life and may require medical intervention. Polycystic Ovary Syndrome (PCOS): A hormonal disorder causing irregular periods, excess androgen levels, and polycystic ovaries. It can lead to infertility and other health issues if not managed properly. Managing Menstrual Health Maintaining menstrual health involves a combination of lifestyle choices, medical care, and self-awareness. Here are some tips for managing menstrual health: Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help regulate hormones and reduce menstrual discomfort. Foods high in omega-3 fatty acids, such as fish and flaxseeds, can also help reduce inflammation. Regular Exercise: Physical activity can alleviate menstrual cramps and improve overall well-being. Activities like yoga, swimming, and walking are particularly beneficial. Stress Management: Practices like yoga, meditation, and deep breathing can help manage stress, which can impact menstrual health. Chronic stress can lead to hormonal imbalances and irregular cycles. Hydration: Drinking plenty of water can reduce bloating and help maintain overall health. Herbal teas, such as chamomile and ginger, can also help alleviate menstrual symptoms. Medical Consultation: Regular check-ups with a healthcare provider can help monitor menstrual health and address any concerns. If you experience severe or persistent symptoms, it’s important to seek medical advice. Menstrual Hygiene Proper menstrual hygiene is crucial for preventing infections and maintaining comfort during menstruation. Here are some tips for menstrual hygiene: Sanitary Products: Use clean and appropriate sanitary products, such as pads, tampons, or menstrual cups. Change them regularly to prevent infections. Menstrual cups and reusable pads are eco-friendly options that can also reduce the risk of irritation. Personal Hygiene: Wash the genital area with mild soap and water. Avoid using harsh chemicals or douches, as they can disrupt the natural balance of bacteria and lead to infections. Disposal: Dispose of used sanitary products properly. Wrap them in paper or a disposal bag before discarding them in a trash bin. Avoid flushing sanitary products down
Understanding Interstitial Lung Disease (ILD)
Understanding Interstitial Lung Disease (ILD) Interstitial Lung Disease (ILD) is a term that encompasses a large group of lung disorders, all of which cause progressive scarring of lung tissue. This scarring can lead to significant breathing problems and reduced oxygen levels in the blood. Let’s delve into the details of ILD, its causes, symptoms, diagnosis, and treatment options. What is Interstitial Lung Disease? Interstitial Lung Disease refers to a collection of over 200 different lung disorders that affect the interstitium, the tissue and space around the air sacs of the lungs. This scarring, or fibrosis, makes the lung tissue stiff, which in turn makes it difficult for the lungs to work properly. Over time, this can lead to serious health issues, including respiratory failure. Causes of Interstitial Lung Disease (ILD) The causes of ILD can be broadly categorized into known and unknown origins: Known Causes: Occupational and Environmental Exposures: Long-term exposure to hazardous materials such as asbestos, silica dust, and coal dust. Medications: Certain drugs, including chemotherapy agents, antibiotics, and heart medications, can cause lung damage. Radiation Therapy: Used in cancer treatment, radiation can lead to lung scarring. Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and scleroderma can cause ILD. Infections: Chronic infections such as hepatitis C and HIV. Unknown Causes: Idiopathic Pulmonary Fibrosis (IPF): The most common form of ILD with no known cause. Symptoms of Interstitial Lung Disease The symptoms of ILD can vary but generally include: Shortness of breath, especially during or after physical activity A dry, persistent cough Fatigue and weakness Unintended weight loss Discomfort or pain in the chest As the disease progresses, symptoms can worsen, leading to severe respiratory issues. Diagnosis of ILD Diagnosing ILD involves a combination of medical history, physical examinations, and various tests: Imaging Tests: High-resolution CT scans and X-rays to detect lung abnormalities. Pulmonary Function Tests: To measure lung capacity and the efficiency of gas exchange. Blood Tests: To identify underlying conditions or infections. Bronchoscopy: A procedure to collect lung tissue samples. Lung Biopsy: In some cases, a surgical biopsy may be necessary to confirm the diagnosis. Treatment Options While there is no cure for ILD, treatments aim to manage symptoms and slow disease progression: Medications: Anti-fibrotic drugs like pirfenidone and nintedanib can help reduce lung scarring. Corticosteroids and immunosuppressants may also be prescribed. Oxygen Therapy: To maintain adequate oxygen levels in the blood. Pulmonary Rehabilitation: Exercise and education programs to improve lung function and overall health. Lung Transplant: In severe cases, a lung transplant may be considered. Living with ILD Living with ILD requires ongoing medical care and lifestyle adjustments: Regular Monitoring: Frequent check-ups with a pulmonologist. Healthy Lifestyle: Eating a balanced diet, staying active, and avoiding smoking. Vaccinations: Staying up-to-date with flu and pneumonia vaccines to prevent respiratory infections. Conclusion Interstitial Lung Disease is a complex and challenging condition, but with proper management and care, individuals can maintain a good quality of life. Early diagnosis and treatment are crucial in slowing the progression of the disease and managing symptoms effectively. For more detailed information and support, consult with healthcare professionals and consider joining support groups for individuals with ILD. Dr. M.V.Sree Keerthi Interventional Pulmonologist View Profile About Author Interventional Pulmonologist M.B.B.S, D.T.C.D (Gold Medalist), DNB (Pulmonary Medicine) , Fellowship in Interventional Pulmonology Dr. M.V.S. Keerthi is a leading pulmonologist renowned for her exceptional skills in pulmonary medicine and her empathetic approach to patient care. Dr. Keerthi is passionate about innovation and lifelong learning, and she is committed to providing her patients with individualized, advanced care. She is a well-respected and trusted individual in respiratory medicine because of her unwavering dedication to quality and collaborative spirit. The finest results for her patients are guaranteed by Dr. Keerthi’s skill and compassion, whether she is managing complicated pulmonary problems or offering everyday care. Book an Appointment
Unveiling the Chest: A Comprehensive Guide to CT Thorax Scans
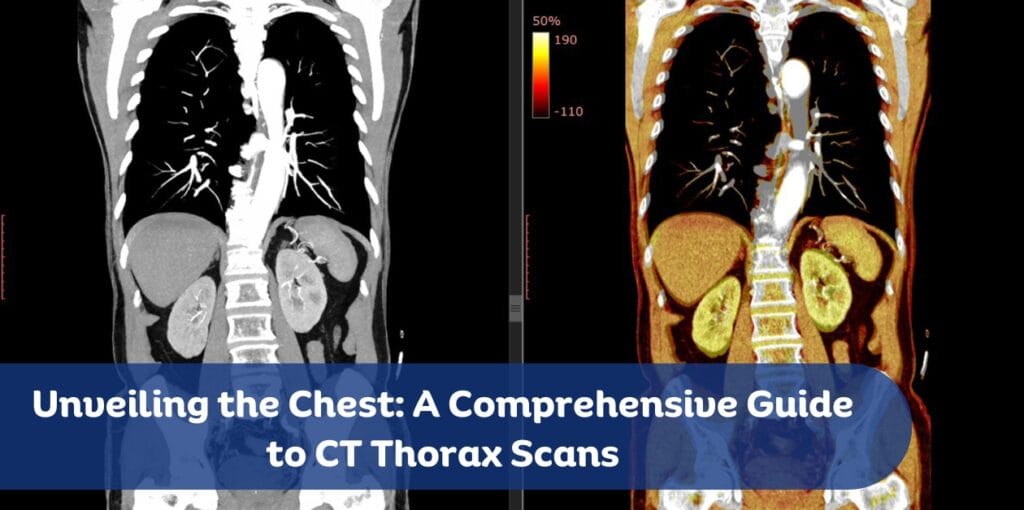
Unveiling the Chest: A Comprehensive Guide to CT Thorax Scans A CT thorax scan, also known as a chest CT scan, is a powerful diagnostic tool that provides detailed images of the chest, including the lungs, heart, blood vessels, and bones. This advanced imaging technique is crucial for diagnosing and monitoring various conditions, offering a clearer picture than standard X-rays. In this blog post, we will explore the importance of CT thorax scans, the procedure, preparation, and what to expect during and after the scan. Understanding CT Thorax Scans A CT (computed tomography) thorax scan uses X-rays and computer technology to create cross-sectional images of the chest. These images provide detailed information about the structures within the chest, allowing healthcare providers to diagnose and monitor a wide range of conditions. The scan can detect abnormalities that may not be visible on a standard chest X-ray, making it an invaluable tool in modern medicine. Why You Might Need a CT Thorax Scan There are several reasons why a healthcare provider might recommend a CT thorax scan: Detecting Infections: CT scans can identify lung infections such as pneumonia, tuberculosis, and fungal infections. They provide detailed images that help in assessing the extent and severity of the infection. Evaluating Injuries: After trauma to the chest, a CT scan can reveal injuries to the lungs, ribs, heart, and blood vessels. This is crucial for determining the appropriate treatment plan. Diagnosing Diseases: CT scans are essential for diagnosing lung cancer, pulmonary embolism, and other lung diseases. They can detect tumors, blood clots, and other abnormalities with high precision. Monitoring Conditions: For chronic conditions like pulmonary fibrosis, chronic obstructive pulmonary disease (COPD), and interstitial lung disease, CT scans help track disease progression and response to treatment. Guiding Procedures: CT scans assist in guiding biopsies and other interventional procedures by providing precise images of the target area. Preparing for the Scan Preparation for a CT thorax scan is generally straightforward, but it may vary depending on whether a contrast dye will be used. Here are some common preparation steps: Dietary Restrictions: If a contrast dye is used, you may be asked to avoid eating or drinking for a few hours before the scan. This helps reduce the risk of nausea and ensures clear images. Medications: Continue taking your regular medications unless instructed otherwise by your healthcare provider. Inform your provider about any allergies, especially to iodine or contrast dye. Clothing and Accessories: Wear comfortable clothing and remove any metal objects, such as jewelry, eyeglasses, and hairpins, as they can interfere with the imaging process. During the Scan The CT thorax scan procedure is quick and painless. Here’s what you can expect: Arrival: Upon arrival at the imaging center, you will check in and provide any necessary medical history. You may be asked to sign a consent form. Preparation: You may need to change into a hospital gown and remove any metal objects. If a contrast dye is used, it may be administered orally or through an intravenous (IV) line. Positioning: You will lie on a motorized table that slides into the CT scanner, a large machine with a tunnel in the center. The technologist will position you correctly and may use straps or pillows to help you stay still. Scanning: The technologist will operate the scanner from a separate room but will be able to see, hear, and speak with you throughout the procedure. You may be asked to hold your breath for short periods to ensure clear images. The scan itself usually takes just a few minutes, although the entire process may take about 30 minutes. After the Scan Once the scan is complete, you can typically resume your normal activities. If a contrast dye was used, you might be advised to drink plenty of fluids to help flush it out of your system. Your healthcare provider will review the images and discuss the results with you, which can help guide further treatment or diagnostic steps. Understanding the Results The images from a CT thorax scan are interpreted by a radiologist, a doctor specialized in reading and analyzing medical images. The radiologist will send a report to your healthcare provider, who will discuss the findings with you. The results can reveal a variety of conditions, including: Lung Diseases: Such as pneumonia, tuberculosis, lung cancer, and COPD. Heart Conditions: Including heart enlargement, pericardial effusion, and congenital heart defects. Blood Vessel Abnormalities: Such as pulmonary embolism, aortic aneurysm, and vascular malformations. Bone and Soft Tissue Issues: Including rib fractures, spinal abnormalities, and soft tissue masses. Risks and Considerations While CT thorax scans are generally safe, there are some risks and considerations to keep in mind: Radiation Exposure: CT scans involve exposure to a small amount of radiation. While the risk is minimal, it is important to discuss any concerns with your healthcare provider, especially if you are pregnant or have had multiple scans. Allergic Reactions: Some people may have allergic reactions to the contrast dye used in CT scans. Inform your healthcare provider if you have a history of allergies to iodine or contrast materials. Kidney Function: The contrast dye can affect kidney function, particularly in individuals with pre-existing kidney conditions. Your healthcare provider may perform blood tests to check your kidney function before administering the dye. Advances in CT Technology Advancements in CT technology have significantly improved the quality and safety of thorax scans. Modern CT scanners use lower doses of radiation while providing high-resolution images. Additionally, new techniques such as dual-energy CT and 4D CT offer enhanced imaging capabilities, allowing for better diagnosis and treatment planning. Conclusion A CT thorax scan is a vital diagnostic tool that provides detailed images of the chest, helping healthcare providers diagnose and monitor a wide range of conditions. Understanding the procedure, preparation, and what to expect can help alleviate any concerns and ensure a smooth experience. With ongoing advancements in CT technology, these scans continue to play a crucial role in modern medicine, offering hope and clarity to patients
Breathless Battles: Conquering pulmonary hypertension disease with Strength and Hope
Pulmonary hypertension (PH) is a chronic and progressive disease that affects the arteries in the lungs and the right side of the heart. It is characterized by high blood pressure in the pulmonary arteries, which can lead to heart failure if left untreated. This blog post aims to shed light on the complexities of pulmonary hypertension, the journey of those affected, and the advancements in treatment that offer hope. Understanding Pulmonary Hypertension Pulmonary hypertension occurs when the blood vessels in the lungs become narrowed, blocked, or destroyed. This makes it harder for blood to flow through the lungs, raising the pressure within the pulmonary arteries. The heart must work harder to pump blood through these arteries, which can eventually weaken the heart muscle. Causes and Symptoms The causes of pulmonary hypertension can be diverse, ranging from genetic predispositions to underlying health conditions such as chronic obstructive pulmonary disease (COPD), heart disease, or autoimmune diseases like scleroderma. In some cases, the cause remains unknown, a condition referred to as idiopathic pulmonary hypertension. Common symptoms include: Shortness of breath, especially during physical activity Fatigue Dizziness or fainting spells Chest pain Swelling in the ankles, legs, and abdomen (edema) Bluish color to the lips and skin (cyanosis) The Diagnosis Journey Diagnosing pulmonary hypertension can be challenging due to its nonspecific symptoms that often mimic other conditions. The diagnostic process typically involves a series of tests, including echocardiograms, chest X-rays, pulmonary function tests, and right heart catheterization, which measures the pressure in the pulmonary arteries. Living with Pulmonary Hypertension Living with pulmonary hypertension requires a multifaceted approach to manage symptoms and improve quality of life. Patients often need to make significant lifestyle changes, including adopting a heart-healthy diet, engaging in appropriate physical activity, and avoiding high altitudes and strenuous activities that can exacerbate symptoms. Emotional and Mental Health The emotional toll of living with a chronic illness like pulmonary hypertension can be substantial. Patients may experience anxiety, depression, and feelings of isolation. Support groups and counseling can be invaluable resources, providing a sense of community and shared understanding. Latest Treatments and Research Advancements in medical research have led to the development of various treatments that can help manage pulmonary hypertension and improve patient outcomes. These treatments include: Medications: Vasodilators, endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and soluble guanylate cyclase stimulators are among the drugs used to relax blood vessels and reduce pressure in the pulmonary arteries. Oxygen Therapy: Supplemental oxygen can help alleviate symptoms and improve oxygen levels in the blood. Surgical Options: In severe cases, procedures such as atrial septostomy or lung transplantation may be considered. One of the most promising developments in recent years is the approval of new medications that target specific pathways involved in the disease process. For example, sotatercept, a novel drug, has shown significant potential in clinical trials by improving exercise capacity and reducing pulmonary vascular resistance. Caregiver Support Caregivers play a crucial role in the lives of pulmonary hypertension patients. They provide physical, emotional, and logistical support, often navigating complex medical systems and advocating for their loved ones. Resources and support groups for caregivers can help them manage their responsibilities and maintain their well-being. Impact of Lifestyle Changes Lifestyle modifications can have a profound impact on managing pulmonary hypertension. Patients are encouraged to: Quit Smoking: Smoking cessation is critical as smoking can worsen symptoms and accelerate disease progression. Healthy Diet: A diet low in salt and rich in fruits, vegetables, and lean proteins can help manage symptoms and improve overall health. Regular Exercise: While strenuous exercise is not recommended, light to moderate physical activity, such as walking or swimming, can be beneficial. Navigating Healthcare Navigating the healthcare system can be daunting for pulmonary hypertension patients and their families. Finding specialists, understanding treatment options, and managing insurance can be overwhelming. Patients are advised to seek care from a multidisciplinary team that includes pulmonologists, cardiologists, and other specialists experienced in treating pulmonary hypertension. Advocacy and Awareness Raising awareness about pulmonary hypertension is essential for improving patient outcomes and advancing research. Advocacy efforts can help secure funding for research, influence policy changes, and provide education to the public and healthcare professionals. Patients and their families can get involved by participating in awareness campaigns, fundraising events, and support groups. Technological Advances Technology is playing an increasingly important role in the management of pulmonary hypertension. Telemedicine allows patients to consult with specialists from the comfort of their homes, while wearable health devices can monitor vital signs and detect early changes in health status. These innovations are making it easier for patients to manage their condition and stay connected with their healthcare team. Conclusion Pulmonary hypertension is a challenging and life-altering disease, but with the right support, treatment, and lifestyle changes, patients can lead fulfilling lives. Continued research and advancements in medical technology offer hope for better treatments and, ultimately, a cure. By raising awareness and advocating for those affected, we can make a significant impact on the lives of pulmonary hypertension patients and their families. Dr. A. Venugopal Clinical Director & HOD Medical Oncology Senior Consultant Medical Oncologist & Hemato-Oncologist View Profile About Author Dr. A. Venugopal MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland). Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology. Book an Appointment
Detecting Cancer Through Blood Tests: An In-Depth Guide

Blood tests have become an essential tool in the early detection and management of cancer. While not all cancers can be detected through blood tests alone, these tests can provide critical information that helps in diagnosing and monitoring the disease. This blog will explore the various types of blood tests used in cancer detection, their benefits, limitations, and the latest advancements in this field. Types of Blood Tests for Cancer Detection 1. Complete Blood Count (CBC) Purpose: A CBC measures the levels of different blood cells, including red blood cells, white blood cells, and platelets. Cancer Detection: Abnormal levels of these cells can indicate blood cancers such as leukemia and lymphoma. For example, a high white blood cell count might suggest leukemia, while low red blood cell counts could indicate anemia caused by cancer. 2. Tumor Marker Tests Purpose: These tests measure the levels of specific proteins or substances produced by cancer cells. Common Markers: Prostate-Specific Antigen (PSA): Elevated levels can indicate prostate cancer. Cancer Antigen 125 (CA 125): High levels may suggest ovarian cancer. Carcinoembryonic Antigen (CEA): Used to monitor colorectal cancer. Limitations: Tumor markers are not definitive for cancer diagnosis as they can also be elevated in non-cancerous conditions. 3. Blood Protein Tests Purpose: These tests, such as electrophoresis, analyze the proteins in the blood. Cancer Detection: They can help diagnose multiple myeloma by identifying abnormal proteins produced by cancerous plasma cells. 4. Circulating Tumor Cell (CTC) Tests Purpose: These tests detect cancer cells that have broken away from the primary tumor and are circulating in the bloodstream. Usage: Primarily used for monitoring the spread of cancers like breast, colon, and prostate cancer. 5. Liquid Biopsies Purpose: A liquid biopsy tests for fragments of DNA from cancer cells in the blood. Advancements: This non-invasive test can detect genetic mutations and help in tailoring personalized treatment plans. Benefits of Blood Tests in Cancer Detection Early Detection: Blood tests can detect cancer at an early stage, which is crucial for successful treatment. Non-Invasive: Most blood tests are minimally invasive compared to traditional biopsies. Monitoring: They are useful for monitoring the effectiveness of treatment and detecting recurrences. Guiding Treatment: Blood tests can provide information about the genetic makeup of the cancer, helping doctors choose the most effective treatments. Limitations and Challenges Not Definitive: Blood tests alone cannot definitively diagnose most cancers. They are usually part of a broader diagnostic process that includes imaging and tissue biopsies. False Positives/Negatives: There is a risk of false positives (indicating cancer when there is none) and false negatives (failing to detect cancer). Variability: Normal ranges for blood test results can vary between individuals, making interpretation challenging. Latest Advancements in Blood Tests for Cancer 1. Multi-Cancer Early Detection (MCED) Tests Innovation: These tests can detect multiple types of cancer from a single blood sample by analyzing DNA and proteins from cancer cells. Potential: They hold promise for early detection of cancers that are currently hard to diagnose early, such as pancreatic and ovarian cancers. 2. Genomic Testing Advancement: Genomic tests analyze the genetic material of cancer cells found in the blood, providing insights into the mutations driving the cancer. Application: This information can be used to develop targeted therapies that are more effective and have fewer side effects. 3. Artificial Intelligence (AI) and Machine Learning Role: AI and machine learning algorithms are being developed to analyze blood test results more accurately and predict cancer risk. Impact: These technologies can improve the accuracy of blood tests and help in early detection and personalized treatment planning. Conclusion Blood tests are a valuable tool in the detection and management of cancer. While they have limitations and are not a standalone diagnostic method, they provide critical information that can guide further testing and treatment. Advances in technology, such as liquid biopsies and multi-cancer early detection tests, are enhancing the capabilities of blood tests, making them more accurate and comprehensive. As research continues, the role of blood tests in cancer detection is likely to expand, offering hope for earlier diagnosis and better outcomes for patients. Dr. A. Venugopal Clinical Director & HOD Medical Oncology Senior Consultant Medical Oncologist & Hemato-Oncologist View Profile About Author Dr. A. Venugopal MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland). Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology. Book an Appointment
The Cancer Genome Atlas (TCGA): Revolutionizing Cancer Research

The Cancer Genome Atlas (TCGA) is a groundbreaking initiative that has transformed our understanding of cancer. Launched in 2006 as a collaborative effort between the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI), TCGA aimed to create a comprehensive “atlas” of the genomic changes involved in cancer. By systematically characterizing the genomic alterations in over 20,000 primary cancer and matched normal samples across 33 different cancer types, TCGA has provided invaluable insights into the molecular mechanisms of cancer, paving the way for advancements in diagnosis, treatment, and prevention. Objectives and Achievements TCGA’s primary goal was to generate a detailed map of the genomic changes that drive cancer. This ambitious project has achieved several key milestones: Massive Data Generation: TCGA produced over 2.5 petabytes of genomic, epigenomic, transcriptomic, and proteomic data. This vast amount of data has been made publicly available, enabling researchers worldwide to access and utilize it for their studies. Improved Cancer Classification: The data generated by TCGA has led to the identification of new cancer subtypes and potential drug targets. By understanding the specific genetic alterations associated with different cancer types, researchers can develop more targeted and effective therapies. Enhanced Diagnostic and Treatment Approaches: Insights from TCGA have contributed to the development of better diagnostic tools and personalized treatment strategies. By tailoring treatments to the genetic profile of individual tumors, clinicians can improve patient outcomes and reduce the side effects of therapy. Key Components of TCGA TCGA’s success can be attributed to several key components: Data Collection and Analysis: TCGA collected samples from various cancer types and used advanced sequencing technologies to analyze them. This comprehensive approach allowed researchers to identify the genetic mutations and alterations that drive cancer. Public Data Access: One of TCGA’s most significant contributions is the public availability of its data through the Genomic Data Commons (GDC) Data Portal. This open-access resource has democratized cancer research, allowing scientists from around the world to explore and analyze the data. Pan-Cancer Atlas: The Pan-Cancer Atlas is a collection of cross-cancer analyses that explore overarching themes such as cell-of-origin patterns and oncogenic processes. This integrative approach has provided a deeper understanding of the commonalities and differences among various cancer types. Impact on Cancer Research TCGA has had a profound impact on cancer research, leading to numerous discoveries and advancements: Identification of Genetic Mutations: TCGA has identified key genetic mutations that drive various cancers. For example, mutations in the BRCA1 and BRCA2 genes are associated with an increased risk of breast and ovarian cancer, while mutations in the TP53 gene are linked to Li-Fraumeni syndrome, which increases the risk of multiple cancer types. Understanding Tumor Biology: The comprehensive data generated by TCGA has improved our understanding of tumor biology and the molecular mechanisms underlying cancer. By studying the genetic alterations in different cancer types, researchers can identify the pathways and processes that contribute to tumor development and progression. Facilitating Collaborative Research: By making its data publicly available, TCGA has fostered collaboration among researchers, accelerating the pace of cancer research. Scientists can build on the findings of TCGA to develop new hypotheses, design experiments, and validate their results. Future Directions Although TCGA officially concluded in 2018, its legacy continues. The data generated by TCGA remains a valuable resource for ongoing research, and new projects are building on TCGA’s foundation to further explore cancer genomics. Some of the future directions in cancer research include: Next-Generation Sequencing: Advances in next-generation sequencing technologies are enabling more detailed and comprehensive analyses of cancer genomes. These technologies allow researchers to identify rare mutations and structural variations that may contribute to cancer. Liquid Biopsies: Liquid biopsies are non-invasive tests that analyze genetic material from blood samples. These tests offer a less invasive alternative to traditional biopsies and can provide real-time information about tumor dynamics and treatment response. CRISPR and Gene Editing: Advances in gene editing technologies like CRISPR hold the potential for correcting genetic mutations and preventing cancer at the genetic level. Researchers are exploring the use of CRISPR to target and modify cancer-causing genes, offering new avenues for treatment and prevention. Ethical and Legal Considerations The use of genetic information in cancer research raises several ethical and legal considerations: Informed Consent: It is essential that individuals fully understand the potential risks and benefits of genetic testing before undergoing the procedure. Informed consent ensures that participants are aware of how their genetic information will be used and the implications of the results. Privacy and Confidentiality: Protecting the privacy and confidentiality of genetic information is crucial to prevent discrimination and misuse. Researchers and healthcare providers must implement robust safeguards to ensure that genetic data is secure and used responsibly. Insurance and Employment: There are concerns about the potential for genetic discrimination in insurance and employment. Laws such as the Genetic Information Nondiscrimination Act (GINA) in the United States provide protections against discrimination based on genetic information, but ongoing vigilance is needed to ensure these protections are upheld. Support and Resources There are numerous resources available for individuals considering genetic testing and those affected by cancer: Genetic Counselors: Genetic counselors are healthcare professionals who provide guidance and support throughout the genetic testing process. They help individuals understand their risk of cancer, interpret test results, and make informed decisions about their health. Support Groups: Many organizations offer support groups for individuals undergoing genetic testing and their families. These groups provide a platform for sharing experiences, offering emotional support, and accessing resources. Educational Resources: Websites, books, and other materials can provide valuable information about genetic testing and cancer risk. Organizations such as the National Cancer Institute (NCI) and the American Cancer Society (ACS) offer comprehensive resources on their websites. Conclusion The Cancer Genome Atlas has been a game-changer in the field of cancer research. By providing a detailed map of the genomic changes in cancer, TCGA has paved the way for advancements in diagnosis, treatment, and prevention. Its impact will continue to be felt for years to come as researchers delve deeper into the
