Thyroid Disease in Women: Early Signs You Shouldn’t Ignore
Thyroid Disease in Women: Early Signs You Shouldn’t Ignore The thyroid is a small, butterfly-shaped gland located in the neck, but its impact on the body is anything but small. It plays a vital role in regulating your metabolism, energy levels, and even mood. For women, thyroid issues are far more common and can often go unnoticed until they cause serious health concerns. At Pi Health Hospital, we believe that awareness is the first step to better health. That’s why we’re highlighting the early warning signs of thyroid disease that women should never ignore. Why Thyroid Health Matters for Women Women are five to eight times more likely than men to develop thyroid disorders. Hormonal changes during puberty, pregnancy, and menopause can significantly affect thyroid function, leading to conditions like hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid). Early Symptoms of Thyroid Disease in Women While symptoms can vary depending on the type of thyroid disorder, here are some of the most common early signs: 1. Unexplained Weight Changes A sudden gain or loss in weight without changes in diet or exercise can be an early indicator of thyroid imbalance. 2. Fatigue or Insomnia Thyroid disorders can affect your sleep patterns, leading to constant tiredness or difficulty sleeping. 3. Menstrual Irregularities Heavy, light, or irregular periods may be linked to thyroid dysfunction, especially during key hormonal phases in life. 4. Mood Swings and Depression Changes in thyroid hormone levels can impact mood, causing anxiety, depression, or irritability. 5. Hair Thinning and Dry Skin An underactive thyroid may slow cell regeneration, resulting in dry, flaky skin and noticeable hair thinning. 6. Sensitivity to Cold or Heat Feeling unusually cold or hot compared to others could signal thyroid problems. 7. Neck Swelling or Discomfort Any swelling or lump in the neck may indicate an enlarged thyroid (goiter), and should be evaluated by a healthcare professional. When to See a Doctor If you’re experiencing one or more of these symptoms, it’s essential to consult a physician. At Pi Health Hospital, our endocrinology experts use advanced diagnostics to assess thyroid health and provide personalized treatment plans. How Pi Health Hospital Can Help Our dedicated team at Pi Health Hospital offers: Comprehensive thyroid screenings Blood tests for TSH, T3, and T4 levels Ultrasound imaging and fine-needle aspiration (FNA) Customized treatment plans including medication and lifestyle guidance Take Control of Your Thyroid Health Today Don’t let thyroid disease disrupt your life. Early detection and treatment are key. Schedule your thyroid check-up at Pi Health Hospital and take the first step toward better health and well-being. Dr. Sarada Kaki Gynaecologist View Profile About Author Dr. Sarada Kaki MBBS, MD – Obstetrics & Gynaecology, DGO, MRCOG (UK) Dr. Sarada Kaki is a highly experienced Gynecologist and Obstetrician, currently practicing at PI Health Cancer Hospital, Gachibowli, Hyderabad. With over 40 years of expertise, she offers comprehensive care in obstetrics and gynecology. She completed her MBBS from Nagarjuna University in 1984 and earned her MD in Obstetrics & Gynaecology from Andhra University in 1987. Dr. Sarada provides a range of specialized services including Pre and Post Delivery Care, Embryo Donor Programs, Pap Smear tests, Lamaze Classes, and Medical Termination of Pregnancy (MTP), ensuring personalized and compassionate care for women at all stages. He is dedicated to offering personalized treatment plans that are tailored to each patient’s unique needs, ensuring optimal outcomes and quality of life. Book an Appointment
Excellence in Head and Neck Oncologic Surgery at PI Health Cancer Hospital In 2025
Excellence in Head and Neck Oncologic Surgery at PI Health Cancer Hospital When it comes to battling complex cancers, having access to specialized care can make all the difference. At PI Health Cancer Hospital, our commitment to world-class cancer treatment is exemplified by our leadership in head and neck oncologic surgery. This highly specialized field focuses on diagnosing and treating tumors in the mouth, throat, larynx, nose, sinuses, and mouth—areas essential to breathing, speaking, and eating What Is Head and Neck Oncologic Surgery? Head and neck oncologic surgery refers to the surgical management of benign and malignant tumors in the head and neck region. This includes cancers of the oral cavity, pharynx, larynx, nasal cavity, salivary glands and thyriod. The goal is not only to remove the cancer but also to preserve function and appearance as much as possible. At PI Health Cancer Hospital, our surgeons are trained in advanced techniques that ensure precise tumor removal with minimal impact on surrounding tissues. Why Choose PI Health Cancer Hospital? Our hospital is a center of excellence for head and neck oncologic surgery. We offer: A multidisciplinary team approach combining surgery, radiation, and medical oncology. Minimally invasive and robotic-assisted surgical options for better recovery outcomes. State-of-the-art imaging and diagnostic tools for accurate treatment planning. Patients at PI Health benefit from personalized treatment plans that optimize cancer control and quality of life. Innovation Meets Compassion Innovation drives our approach to head and neck oncologic surgery. We use cutting-edge technology like intraoperative navigation, endoscopic techniques, and precision-based reconstructions. More importantly, our team prioritizes compassionate care, guiding patients through every step of their journey—from diagnosis to rehabilitation. Our dedicated speech and swallowing therapists, nutritionists, and psychologists work closely with surgical teams to ensure holistic healing. Early Detection Saves Lives Early intervention in cancers requiring head and neck oncologic surgery greatly improves survival rates. If you notice persistent throat pain, hoarseness, difficulty swallowing, or unexplained lumps in the neck, consult a specialist immediately. Our diagnostic experts are skilled in identifying early signs and tailoring prompt treatment strategies Success Stories that Inspire We take pride in the hundreds of successful head and neck oncologic surgery procedures performed at PI Health Cancer Hospital. Our patients go on to lead fulfilling lives, with restored function and renewed confidence. Their stories are a testament to the skill and dedication of our surgical team. Schedule a Consultation Today If you or a loved one needs expert care, trust the specialists in head and neck oncologic surgery at PI Health Cancer Hospital. Our mission is to provide safe, effective, and compassionate treatment tailored to your needs. Dr. Raghu Rami Reddy S Surgical Oncology View Profile About Author Dr. Raghu Rami Reddy S M.B.B.S, M.S, DRNB Surgical Oncology, FALS – Oncology Dr. Raghu Rami Reddy is a highly skilled and experienced Surgical Oncologist specializing in the diagnosis and treatment of various cancers. With a commitment to providing the highest standard of care, Dr. Reddy utilizes advanced surgical techniques to treat a wide range of oncological conditions, including breast, gastrointestinal, and head and neck cancers, among others. He is dedicated to offering personalized treatment plans that are tailored to each patient’s unique needs, ensuring optimal outcomes and quality of life. Book an Appointment
The Role of Platelets in Dengue Recovery: Myth vs. Fact
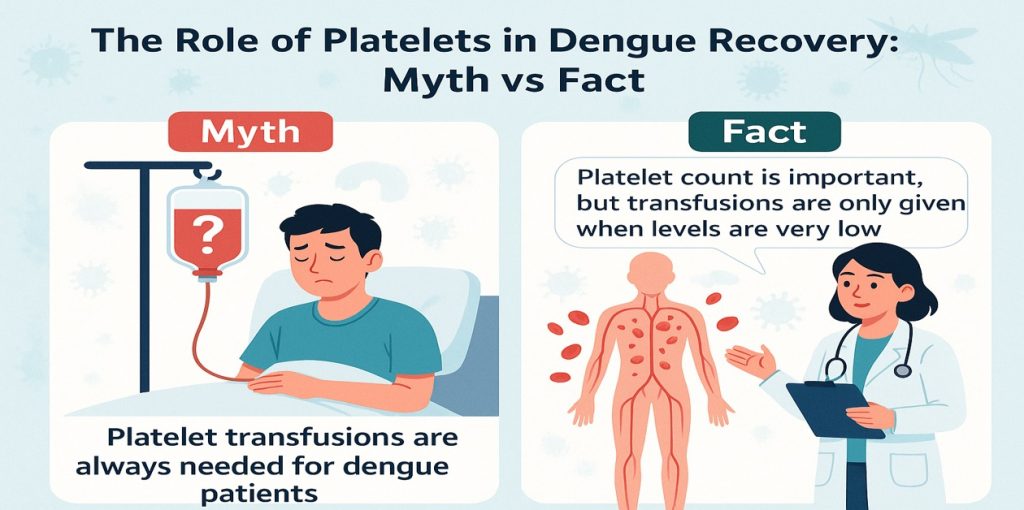
The Role of Platelets in Dengue Recovery: Myth vs. Fact When someone is diagnosed with dengue fever, one word instantly becomes the center of every conversation: platelets. From family members anxiously refreshing lab reports to social media posts suggesting miracle cures, there’s a whirlwind of information (and misinformation) surrounding this crucial blood component. But how vital are platelets in dengue recovery? Let’s dive into the facts, bust the myths, and highlight where you can get the best treatment. What Are Platelets, and Why Do They Matter? Platelets are small, colorless cell fragments in your blood whose main job is to stop bleeding by clumping and clotting at the site of injury. In the context of dengue, a mosquito-borne viral infection, platelets play a crucial role in monitoring the disease’s severity. When infected with the dengue virus, many patients experience a drop in platelet count. This phenomenon, known as thrombocytopenia, often triggers panic—but it’s not always as alarming as it seems. Understanding when a low platelet count becomes critical is key to handling dengue effectively. Common Myths vs. Medical Facts Let’s set the record straight by looking at some of the most widespread myths versus the actual medical truths. Myth 1: Low Platelets Always Require Transfusion One of the most persistent myths is that a drop in platelet count automatically warrants a transfusion. In reality, doctors evaluate more than just numbers—they look at symptoms, bleeding risk, and overall patient stability. Most dengue patients recover without ever needing a transfusion. Fact: Platelet transfusions are only recommended when the count falls below 10,000–20,000 and there’s active or high-risk bleeding. Myth 2: Eating Certain Foods Can Instantly Boost Platelets Papaya leaf juice, kiwi, pomegranate, goat milk—you’ve probably heard of these being touted as natural platelet boosters. While these foods are nutritious and support overall immunity, there’s no scientific proof they directly or instantly increase platelets. Fact: A well-balanced diet supports recovery, but no food alone can restore platelet levels immediately. Rely on medical advice, not viral remedies. Myth 3: The Lower the Platelets, the Worse the Outcome Another misconception is that a low platelet count directly determines the severity of dengue. However, many patients with low platelets recover fully without complications, while others with higher counts may still face risks if other symptoms worsen. Fact: Doctors assess dengue severity based on various factors—platelet count is just one of them. The Role of Monitoring and Medical Supervision Monitoring platelet count is essential in dengue, but it’s not the only metric. Doctors also look at hematocrit levels, liver function, and signs of internal bleeding. Panicking over a number without clinical symptoms can lead to unnecessary stress and even overtreatment. That’s why it’s so important to get expert guidance from a trusted healthcare provider. Best Dengue Care at PI Health Hospital When it comes to managing dengue and tracking platelets, experience and precision matter. At PI Health Hospital, patients receive comprehensive care that goes beyond numbers. From skilled doctors and 24/7 lab monitoring to compassionate nursing and advanced treatment options, you’re in safe hands every step of the way. Why choose PI Health Hospital? Expert haematology and infectious disease specialists Accurate and timely platelet monitoring Personalized dengue treatment protocols Emergency care for critical cases Proven patient recovery outcomes When you’re dealing with a condition as sensitive as dengue, you want to be in a place where the focus isn’t just on lab results—but on total patient care. That’s what PI Health Hospital delivers, every time. Final Takeaway In the battle against dengue, knowledge is power. Platelets are important, but they’re not the whole story. Don’t fall for myths and misinformation—trust verified medical advice and get the care you need from the experts. If you or a loved one is facing dengue, don’t delay. Visit PI Health Hospital for the best dengue care and expert guidance on platelet management. Because real recovery starts with real care. Dr. Y Swetha Consultant General Physician View Profile About Author Dr. Y Swetha MBBS , MD (General Medicine) Dr. Y Swetha is a skilled physician currently practicing at PI Health Cancer Hospital. She holds an MBBS from Kamineni Institute of Medical Sciences and an MD in General Medicine from Prathima Institute of Medical Sciences. Dr. Swetha has extensive experience in outpatient, inpatient, emergency, and critical care settings. She is proficient in managing chronic conditions, critical emergencies, and advanced procedures such as ventilator management and catheter placements. Book an Appointment
Best Affordable Head and Neck Cancer Hospital – Pi Health Cancer Hospital
Best Affordable Head and Neck Cancer Hospital – Pi Health Cancer Hospital When it comes to fighting head and neck cancer, finding the right hospital is a crucial decision. Patients not only look for expert care but also for a treatment option that is affordable without compromising on quality. At Pi Health Cancer Hospital, we take pride in being one of the best affordable head and neck cancer hospitals in India, offering advanced surgical treatments with compassion and precision. Why Choose Pi Health for Head and Neck Cancer Surgery? At Pi Health, our mission is clear: to provide affordable cancer care backed by state-of-the-art technology and a team of highly skilled oncologists and surgeons. We believe that quality healthcare should be accessible to everyone, regardless of their financial background. 👨⚕️ Expert Surgical Team Our team of head and neck cancer specialists has performed hundreds of successful surgeries. From early-stage tumors to complex cases, our surgeons use the latest techniques to ensure the best outcomes. 💰 Truly Affordable Care Unlike many hospitals that charge exorbitant fees, Pi Health ensures every patient receives affordable care. We offer transparent pricing, no hidden charges, and treatment packages that are tailored to suit your budget. Whether you’re looking for surgery, chemotherapy, or radiation therapy, we make sure it’s all within reach. 🏥 Advanced Facilities We are equipped with cutting-edge diagnostic tools, surgical equipment, and post-operative care units. Our infrastructure rivals the best in the country, yet our treatment remains affordable for all. What Makes Us the Best Affordable Hospital? Customizable treatment plans to suit different financial needs Government insurance and health schemes supported Free initial consultations on select days Special discounts for senior citizens and economically weaker patients Our patient-first approach, combined with affordable pricing, is why people from across India—and even abroad—choose Pi Health for their head and neck cancer surgery. Our Surgical Expertise We are proud to offer: Microsurgical reconstruction for complex defects Nerve-sparing procedures to preserve voice and swallowing function Advanced preoperative imaging and 3D planning tools for precision Every patient receives a tailored head and neck surgery plan that considers both clinical needs and personal preferences. Our expertise in head and neck surgery ensures that you receive care that’s not only effective but also focused on long-term wellness and quality of life. Recovery and Support Post-surgical care is critical to recovery. Our multidisciplinary team offers: Speech and swallowing rehabilitation Nutritional counseling Pain management Emotional and psychological support We understand that head and neck surgery is more than just a medical procedure—it’s a life-changing experience. From diagnosis through recovery, you’re not alone. We walk this journey with you—every step of the way. Why Choose PI Health Cancer Hospital? With a combined experience, state-of-the-art facilities, and a patient-first approach, PI Health Cancer Hospital stands at the forefront of head and neck surgery. Our commitment goes beyond curing the disease—we aim to restore quality of life and empower our patients to live fully Dr. Raghu Rami Reddy S Surgical Oncology View Profile About Author Dr. Raghu Rami Reddy S M.B.B.S, M.S, DRNB Surgical Oncology, FALS – Oncology Dr. Raghu Rami Reddy is a highly skilled and experienced Surgical Oncologist specializing in the diagnosis and treatment of various cancers. With a commitment to providing the highest standard of care, Dr. Reddy utilizes advanced surgical techniques to treat a wide range of oncological conditions, including breast, gastrointestinal, and head and neck cancers, among others. He is dedicated to offering personalized treatment plans that are tailored to each patient’s unique needs, ensuring optimal outcomes and quality of life. Book an Appointment
Understanding Head and Neck Cancer Surgery: A Vital Step Toward Healing

Understanding Head and Neck Cancer Surgery: A Vital Step Toward Healing By PI Health Cancer Hospital In 2025 At PI Health Cancer Hospital, we understand that a cancer diagnosis—especially one affecting the head and neck—can be overwhelming. These cancers can impact essential functions such as speaking, breathing, eating, and even facial appearance. That’s why our team of specialists is dedicated to offering the most advanced, compassionate, and personalized head and neck surgery available. What Is Head and Neck Cancer? Head and neck cancers typically begin in the squamous cells lining the moist, mucosal surfaces inside the head and neck, including the mouth, throat, larynx (voice box), nasal cavity, and sinuses. They can also affect the salivary glands,thyriod and lymph nodes. Common risk factors include: Tobacco and alcohol use Human papillomavirus (HPV) infection Prolonged sun exposure (for lip cancer) Poor oral hygiene and certain occupational exposures The Role of Head and Neck Surgery in Treatment Head and neck surgery is often a cornerstone in the treatment of these cancers. Depending on the location and stage of the cancer, surgery may involve: Tumor removal – excising the cancerous tissue while preserving as much healthy tissue as possible Lymph node dissection – removing lymph nodes in the neck to prevent the spread of cancer Reconstructive surgery – rebuilding areas affected by head and neck surgery using tissue grafts or flaps to restore function and appearance Rehabilitation At PI Health Cancer Hospital, our surgical team collaborates closely with reconstructive surgeons, speech therapists, and oncologists to ensure optimal outcomes in both function and aesthetics. Our Surgical Expertise We are proud to offer: Microsurgical reconstruction for complex defects Nerve-sparing procedures to preserve voice and swallowing function Advanced preoperative imaging and 3D planning tools for precision Every patient receives a tailored head and neck surgery plan that considers both clinical needs and personal preferences. Our expertise in head and neck surgery ensures that you receive care that’s not only effective but also focused on long-term wellness and quality of life. Recovery and Support Post-surgical care is critical to recovery. Our multidisciplinary team offers: Speech and swallowing rehabilitation Nutritional counseling Pain management Emotional and psychological support We understand that head and neck surgery is more than just a medical procedure—it’s a life-changing experience. From diagnosis through recovery, you’re not alone. We walk this journey with you—every step of the way. Why Choose PI Health Cancer Hospital? With a combined experience, state-of-the-art facilities, and a patient-first approach, PI Health Cancer Hospital stands at the forefront of head and neck surgery. Our commitment goes beyond curing the disease—we aim to restore quality of life and empower our patients to live fully Dr. Raghu Rami Reddy S Surgical Oncology View Profile About Author Dr. Raghu Rami Reddy S M.B.B.S, M.S, DRNB Surgical Oncology, FALS – Oncology Dr. Raghu Rami Reddy is a highly skilled and experienced Surgical Oncologist specializing in the diagnosis and treatment of various cancers. With a commitment to providing the highest standard of care, Dr. Reddy utilizes advanced surgical techniques to treat a wide range of oncological conditions, including breast, gastrointestinal, and head and neck cancers, among others. He is dedicated to offering personalized treatment plans that are tailored to each patient’s unique needs, ensuring optimal outcomes and quality of life. Book an Appointment
Colorectal Cancer Awareness Month: Educate, Prevent, and Detect Early – Copy – Copy
Home >> Colorectal Cancer Awareness Month: Educate, Prevent, and Detect Early What is Colorectal Cancer Awareness Month? Colorectal Cancer Awareness Month is observed every March to raise awareness about colorectal cancer, which includes cancers of the colon and rectum. This month is dedicated to educating the public about the importance of early detection, prevention, and treatment. Purpose of Colorectal Cancer Awareness Month The primary goal is to increase awareness about colorectal cancer, the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths in the United States. Early detection through screening can significantly improve survival rates. Importance of Screening for Colorectal Cancer Who Should Get Screened? Regular screening is crucial, especially for individuals aged 45 and older or those with a family history of the disease. Common Screening Methods Colonoscopy Fecal Occult Blood Test (FOBT) Stool DNA Test Understanding the Risk Factors Awareness campaigns often highlight risk factors such as: Age Family history Inflammatory bowel disease Lifestyle factors (e.g., diet, physical inactivity, smoking, and heavy alcohol use) Genetic syndromes Recognizing Symptoms of Colorectal Cancer Educating the public about the symptoms of colorectal cancer is vital. Symptoms can include: Changes in bowel habits Blood in the stool Abdominal discomfort Unexplained weight loss Fatigue However, early stages often have no symptoms, underscoring the importance of screening. Prevention Tips Promoting lifestyle changes can reduce the risk of colorectal cancer. These include: Maintaining a healthy diet rich in fruits, vegetables, and whole grains Regular physical activity Avoiding tobacco Limiting alcohol consumption Advocacy and Support Organizations like the American Cancer Society and the Colorectal Cancer Alliance use this month to: Advocate for policy changes Fundraise for research Provide support to patients and their families Events and Activities Various events are organized to spread the word and encourage people to get screened, including: Walks and runs Educational seminars Social media campaigns The Symbol of Colorectal Cancer Awareness The awareness ribbon for colorectal cancer is dark blue, often displayed during March to show support for those affected by the disease. Conclusion By focusing on education, prevention, and early detection, Colorectal Cancer Awareness Month aims to reduce the incidence and mortality of colorectal cancer and improve the quality of life for those affected by it. Dr. A. Venugopal Clinical Director & HOD Medical Oncology Senior Consultant Medical Oncologist & Hemato-Oncologist View Profile About Author Dr. A. Venugopal MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland). Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology. Book an Appointment
World Malaria Day 2025: Uniting for a Malaria-Free Future

World Malaria Day 2025: Uniting for a Malaria-Free Future Each year on April 25th, the world comes together to mark World Malaria Day, an important occasion dedicated to raising global awareness about malaria — a preventable and curable disease that continues to affect millions, particularly in tropical and subtropical regions. This year’s theme, “Accelerating the Fight Against Malaria,” emphasizes the need for collective action, innovation, and increased investment in healthcare to finally eliminate this disease. At PI Health Hospital, we stand proudly with the global community, contributing actively through healthcare services, education, and prevention programs. Malaria is caused by Plasmodium parasites, transmitted to humans through the bite of an infected Anopheles mosquito. The disease can cause high fever, chills, headache, nausea, and in severe cases, can lead to complications such as organ failure and even death. Though preventable and treatable, malaria still claims over 600,000 lives annually, most of them children under 5 years of age in sub-Saharan Africa. Why World Malaria Day Matters World Malaria Day is not just about information — it’s about action. It reminds us that: Prevention saves lives Early diagnosis reduces complications Community education empowers families Global partnerships drive change How we can make a difference in the Fight Against Malaria As a trusted healthcare provider, PI Health Hospital plays a critical role in combatting malaria at both the clinical and community level. Here’s how we are making a difference: 1. Early Diagnosis and Effective Treatment We provide: Rapid diagnostic tests (RDTs) Microscopy-based detection Affordable and WHO-recommended treatment options Our trained medical professionals ensure prompt and precise care to prevent complications and hospitalizations. 2. Community Awareness & Outreach We believe prevention starts with education. Our teams conduct: School and community awareness programs Public talks on mosquito control and personal protection Distribution of educational materials in local languages 3. Prevention Initiatives Through partnerships and outreach, we distribute: Insecticide-treated mosquito nets (ITNs) Mosquito repellents Leaflets on eliminating stagnant water around homes 4. Health Camps & Screenings In honor of World Malaria Day, we are hosting: Free malaria screenings Outreach health camps Consultations with general physicians and specialists These efforts help in identifying high-risk individuals early and creating awareness about available treatment options. Research and Innovation Our team is also involved in tracking malaria trends and studying resistance to anti-malarial drugs, contributing to broader public health efforts. What You Can Do You can join us in the fight against malaria by taking a few simple steps: Use mosquito nets and repellents Wear long sleeves and cover exposed skin during evenings Remove stagnant water from around your home Get tested immediately if you have fever, chills, or weakness Educate others in your community Together Toward a Healthier Future On World Malaria Day 2025, we at PI Health Hospital recommit ourselves to the goal of a malaria-free world. Our hospital will continue to lead with care, compassion, and innovation, ensuring that no life is lost to a disease that is entirely preventable. Visit us for screening, join our awareness programs, and help us spread the word. With collective effort, malaria can be history. Dr. Y Swetha Consultant General Physician View Profile About Author Dr. Y Swetha MBBS , MD (General Medicine) Dr. Y Swetha is a skilled physician currently practicing at PI Health Cancer Hospital. She holds an MBBS from Kamineni Institute of Medical Sciences and an MD in General Medicine from Prathima Institute of Medical Sciences. Dr. Swetha has extensive experience in outpatient, inpatient, emergency, and critical care settings. She is proficient in managing chronic conditions, critical emergencies, and advanced procedures such as ventilator management and catheter placements. Book an Appointment
Link Between Obesity and Cholesterol : A Guide to a Healthier You

Link Between Obesity and Cholesterol : A Guide to a Healthier You In 2025 Obesity and cholesterol are closely connected health concerns that affect millions globally. Individually, they increase the risk of heart disease, stroke, and type 2 diabetes. Together, they create a silent threat to your long-term well-being. The good news? Both obesity and high cholesterol are manageable — and often reversible — through lifestyle changes, awareness, and medical guidance. In this guide, we’ll explore the link between obesity and cholesterol, signs to watch for, and effective ways to take control of your health. What Is Cholesterol and What Does It Do? Cholesterol is a waxy, fat-like substance found in every cell of the body. It’s essential for many functions, such as: Building cell membranes Producing hormones like estrogen and testosterone Synthesizing vitamin D Creating bile acids that help digest fats Silent But Serious: Symptoms of High Cholesterol High cholesterol is often symptomless — which is why it’s referred to as a “silent” condition. Still, in some cases, you might notice: Chest pain or angina Fatigue or shortness of breath Xanthomas: yellowish fatty deposits under the skin, especially around eyes, elbows, or knees Weight gain or visible abdominal obesity Peripheral vascular disease Because symptoms are rare, the only reliable way to detect high cholesterol is through a simple blood test. The Strong Link Between Obesity and Cholesterol The Strong Link Between Obesity and Cholesterol There’s a direct and powerful connection between obesity and cholesterol levels. Obesity, especially around the abdomen, leads to an unhealthy lipid profile: Increased LDL (bad cholesterol) Decreased HDL (good cholesterol) Elevated triglycerides, another type of fat in the blood This combination drastically raises your risk of cardiovascular disease and metabolic syndrome. How to Manage Cholesterol and Combat Obesity The most effective way to improve both obesity and cholesterol levels is through sustainable lifestyle changes. Here’s what you can do: 1. Healthy Eating Habits Add soluble fiber: oats, beans, apples, and citrus fruits Include healthy fats: avocados, olive oil, nuts, and fatty fish Reduce sugar and refined carbs Avoid trans fats and saturated fats: processed snacks, fried foods, and full-fat dairy Stay hydrated with water instead of sugary drink 2. Regular Physical Activity Aim for 30 minutes of moderate exercise (like brisk walking) at least 5 days a week Add strength training twice a week to build muscle and boost metabolism 3. Weight Management Losing just 5–10% of your body weight can significantly lower cholesterol Focus on long-term habits, not crash diet 4. Quit Smoking and Limit Alcohol Smoking lowers HDL (good cholesterol) and damages your blood vessels Quitting improves heart health almost immediately Reduce alcohol intake to support weight and cholesterol control 5. Prioritize Sleep and Manage Stress Get 7–9 hours of quality sleep every night Practice stress-relieving techniques: meditation, yoga, deep breathing, or journaling Medical Treatments for High Cholesterol When lifestyle changes aren’t enough, your doctor might recommend medications such as: Statins – lower LDL cholesterol Ezetimibe – reduces cholesterol absorption PCSK9 inhibitors – effective for genetic high cholesterol Bile acid sequestrants – help eliminate excess cholesterol Always follow your doctor’s guidance and attend regular check-ups. Conclusion: Your Health Is in Your Hands Obesity and cholesterol may not cause immediate symptoms, but they can gradually damage your heart, blood vessels, and organs. Taking early, proactive steps can make all the difference. Start small: Walk for 10 minutes after meals Choose grilled over fried foods Swap soda for water These tiny shifts add up to massive gains over time. Your body is your lifelong home. Treat it with care — and it will reward you with strength and vitality. Don’t wait for symptoms to appear. Get your cholesterol checked and take the first step toward a healthier future today. Dr. Y Swetha Consultant General Physician View Profile About Author Dr. Y Swetha MBBS , MD (General Medicine) Dr. Y Swetha is a skilled physician currently practicing at PI Health Cancer Hospital. She holds an MBBS from Kamineni Institute of Medical Sciences and an MD in General Medicine from Prathima Institute of Medical Sciences. Dr. Swetha has extensive experience in outpatient, inpatient, emergency, and critical care settings. She is proficient in managing chronic conditions, critical emergencies, and advanced procedures such as ventilator management and catheter placements. Book an Appointment
Recognizing the Symptoms of Multiple Myeloma Early
Recognizing the Symptoms of Multiple Myeloma Early Multiple myeloma, a type of blood cancer, is a rare but serious condition that affects plasma cells in the bone marrow. These cancerous cells interfere with the production of healthy blood cells, which can lead to a variety of symptoms. Because the symptoms of myeloma can be subtle and may overlap with other conditions, early detection is critical for improving treatment outcomes. In this blog, we will explore the key myeloma symptoms, how multiple myeloma is diagnosed, and the importance of early intervention, with a focus on groundbreaking clinical trials at PI Health Cancer Hospital that are advancing the future of cancer detection and treatment. What is Multiple Myeloma? Multiple myeloma is a cancer that begins in plasma cells, a type of white blood cell found in the bone marrow. Plasma cells are responsible for producing antibodies, but in multiple myeloma, these cells become abnormal and proliferate uncontrollably. This leads to a reduction in the production of normal blood cells and can cause damage to bones, kidneys, and the immune system. While multiple myeloma is rare, it is one of the more common types of blood cancer, affecting thousands of people worldwide. The exact cause of myeloma remains unclear, but risk factors such as age, family history, and certain genetic mutations may play a role. Early Symptoms of Multiple Myeloma Recognizing myeloma symptoms early can be challenging, as many of them overlap with other conditions. However, there are certain signs that may indicate the presence of multiple myeloma. These include: Bone Pain or Fractures One of the hallmark signs of multiple myeloma is bone pain, particularly in the back, ribs, or hips. This occurs because the abnormal plasma cells can weaken the bones, making them more prone to fractures. If you experience persistent or unexplained bone pain, it is essential to consult a healthcare provider for further evaluation. Fatigue and Weakness Feeling unusually tired or weak, even after resting, is another common symptom of multiple myeloma. This fatigue is caused by a lack of healthy red blood cells, which can lead to anemia. Anemia can also cause dizziness, shortness of breath, and a general feeling of being unwell. Frequent Infections Because myeloma affects the immune system, individuals with this condition may be more susceptible to frequent infections. This is due to the reduced production of normal antibodies, which weakens the body’s ability to fight off infections. If you find yourself getting sick more often than usual, it may be worth discussing this with your doctor. Kidney Problems Myeloma can also affect the kidneys, as the abnormal proteins produced by the cancerous plasma cells can accumulate in the kidneys and cause damage. Symptoms of kidney problems may include swelling in the legs or ankles, pain in the lower back, and changes in urination patterns. Hypercalcemia (High Calcium Levels) Multiple myeloma can cause elevated levels of calcium in the blood, a condition known as hypercalcemia. This may lead to symptoms such as nausea, vomiting, constipation, confusion, and excessive thirst. If left untreated, hypercalcemia can cause severe complications. The Role of Sun Exposure in Melanoma While anyone can develop melanoma, exposure to ultraviolet (UV) radiation from the sun or tanning beds is one of the leading risk factors for developing skin cancer. UV rays damage the DNA in skin cells, leading to mutations that can result in cancer. It’s important to note that melanoma can occur in areas that are not typically sun-exposed, so even those with limited sun exposure should remain vigilant about skin changes. Additionally, people with fair skin, a history of sunburns, or a family history of skin cancer are at a higher risk. How PI Health Cancer Hospital is Advancing Melanoma Detection and Treatment PI Health Cancer Hospital is at the forefront of melanoma research, conducting groundbreaking clinical trials that focus on innovative methods for early detection and treatment. These clinical trials are exploring new ways to identify melanoma at its earliest stages, allowing for more effective treatments and better outcomes for patients. Clinical Trials Focused on Early Cancer Detection One of the most exciting advancements in melanoma research at PI Health Cancer Hospital is the development of non-invasive screening technologies. These include innovative imaging techniques and molecular markers that can detect melanoma before visible symptoms appear. By identifying melanoma early, doctors can begin treatment while the cancer is still confined to the skin, significantly improving the patient’s prognosis. Immunotherapy and Targeted Treatments In addition to early detection, PI Health Cancer Hospital is also pioneering clinical trials that explore the use of immunotherapy and targeted treatments for melanoma. Immunotherapy works by boosting the body’s natural defenses to recognize and fight cancer cells, while targeted therapies aim at specific genes or proteins that drive cancer growth. These treatments offer promising results for patients with advanced melanoma, and clinical trials are helping to refine their effectiveness. Personalized Cancer Care Another key focus of PI Health Cancer Hospital’s clinical trials is personalized cancer care. By analyzing each patient’s unique genetic makeup, doctors can tailor treatments to the individual’s specific needs. This personalized approach has shown tremendous success in improving treatment outcomes and minimizing side effects. How to Protect Yourself from Melanoma While early detection is essential, prevention is equally important. Here are some tips to help reduce your risk of developing melanoma: Use Sunscreen: Always apply broad-spectrum sunscreen with SPF 30 or higher, even on cloudy days. Reapply every two hours, or more frequently if swimming or sweating. Avoid Tanning Beds: Tanning beds expose the skin to elevated levels of UV radiation, increasing the risk of melanoma. Wear Protective Clothing: When spending time outdoors, wear protective clothing, wide-brimmed hats, and sunglasses to reduce sun exposure. Seek Shade: Avoid prolonged exposure to the sun, especially during peak hours (10 a.m. to 4 p.m.). Regular Skin Checks: Perform regular self-exams of your skin to check for any new or changing moles. Schedule annual checkups with a dermatologist for professional skin evaluations. Conclusion Melanoma is a serious
Colorectal Cancer Awareness Month: Educate, Prevent, and Detect Early
Home >> Colorectal Cancer Awareness Month: Educate, Prevent, and Detect Early What is Colorectal Cancer Awareness Month? Colorectal Cancer Awareness Month is observed every March to raise awareness about colorectal cancer, which includes cancers of the colon and rectum. This month is dedicated to educating the public about the importance of early detection, prevention, and treatment. Purpose of Colorectal Cancer Awareness Month The primary goal is to increase awareness about colorectal cancer, the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths in the United States. Early detection through screening can significantly improve survival rates. Importance of Screening for Colorectal Cancer Who Should Get Screened? Regular screening is crucial, especially for individuals aged 45 and older or those with a family history of the disease. Common Screening Methods Colonoscopy Fecal Occult Blood Test (FOBT) Stool DNA Test Understanding the Risk Factors Awareness campaigns often highlight risk factors such as: Age Family history Inflammatory bowel disease Lifestyle factors (e.g., diet, physical inactivity, smoking, and heavy alcohol use) Genetic syndromes Recognizing Symptoms of Colorectal Cancer Educating the public about the symptoms of colorectal cancer is vital. Symptoms can include: Changes in bowel habits Blood in the stool Abdominal discomfort Unexplained weight loss Fatigue However, early stages often have no symptoms, underscoring the importance of screening. Prevention Tips Promoting lifestyle changes can reduce the risk of colorectal cancer. These include: Maintaining a healthy diet rich in fruits, vegetables, and whole grains Regular physical activity Avoiding tobacco Limiting alcohol consumption Advocacy and Support Organizations like the American Cancer Society and the Colorectal Cancer Alliance use this month to: Advocate for policy changes Fundraise for research Provide support to patients and their families Events and Activities Various events are organized to spread the word and encourage people to get screened, including: Walks and runs Educational seminars Social media campaigns The Symbol of Colorectal Cancer Awareness The awareness ribbon for colorectal cancer is dark blue, often displayed during March to show support for those affected by the disease. Conclusion By focusing on education, prevention, and early detection, Colorectal Cancer Awareness Month aims to reduce the incidence and mortality of colorectal cancer and improve the quality of life for those affected by it. Dr. A. Venugopal Clinical Director & HOD Medical Oncology Senior Consultant Medical Oncologist & Hemato-Oncologist View Profile About Author Dr. A. Venugopal MD (General Medicine), DM (Medical Oncology), MRCP – SCE Medical Oncology (UK), ECMO (Switzerland). Dr A. Venugopal is One of the best medical oncologist and Hemato Oncologist in hyderabad, currently serving as the Head of the Department and Senior Medical Oncologist, Hemato Oncologist at Pi Health Cancer Hospital in Gachibowli, Hyderabad. He brings over 15 years of extensive experience in the field of Oncology. Book an Appointment
